Bioavailability Explained
We often assume that consuming a supplement or nutrient-dense food is enough to unlock its benefits. But the reality is far more nuanced. The concept of bioavailability—the proportion of a nutrient that actually enters circulation and becomes available for biological activity—determines whether a supplement works or simply passes through the body unmetabolized.
So, what are the barriers to bioavailability, and how can we enhance it to maximize health outcomes?
The science of bioavailability - more than just digestion
Bioavailability is not just about how much of a nutrient is consumed, but rather:
- How well it’s absorbed into the bloodstream
- Whether it reaches the target tissues
- How effectively it’s utilized at the cellular level
For example, you might take 100mg of a given nutrient, but only absorb a fraction of that.
Several key factors influence how well the body absorbs and utilizes nutrients:
Molecular structure & solubility:
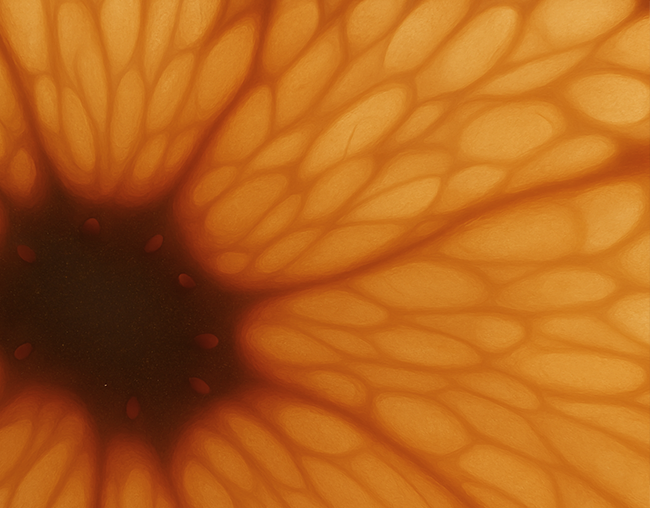
Nutrient absorption begins at the cellular level, where molecular size, solubility, and polarity dictate how easily a compound crosses the intestinal barrier.
For example: Iron exists in heme (animal-based) and non-heme (plant-based) forms, with heme iron being significantly more bioavailable.¹
Your gut health & digestive enzymes:
Nutrients don’t act in isolation—they interact with enzymes, gut bacteria, and metabolic pathways that affect their availability.
For example, polyphenols in native Australian plants (e.g., Kakadu plum, Davidson plum) are metabolized by gut bacteria before they become bioactive.
The gut-liver axis plays a role in first-pass metabolism, where certain compounds are broken down in the gut and then pass through the liver before reaching circulation.
Competing nutrients & interactions:
Certain nutrients compete for absorption or require specific co-factors.
For example, Vitamin C enhances non-heme iron absorption, while calcium inhibits it.
Fats improve the absorption of fat-soluble vitamins (A, D, E, K) and lipophilic compounds like curcumin.
Delivery method: Supplement design impacts absorption.For example:
- Liposomal and nano-emulsified formulations enhance the delivery of fat-soluble compounds.²
- Fermentation and hydrolysis can improve bioavailability by pre-digesting certain compounds.³
- Chelated minerals (e.g., magnesium glycinate vs. magnesium oxide) can offer superior absorption compared to their inorganic counterparts.⁴ ⁵
The Problem: not all nutrients are created equal
When evaluating supplements, formulation matters. Some forms of vitamins and minerals are superior in absorption and utilization, while others are cheap, poorly absorbed, or cause unwanted side effects.
Examples of key differences in formulation:
Folate: Folic Acid vs. Methylfolate
⦁ Folic acid must be converted to the biologically active form of folate (L-methylfolate) by the MTHFR enzyme before the body can use it.
⦁ L-methylfolate (5-MTHF) is already in the biologically active form, making it immediately bioavailable— This means it has been suggested as an alternative way to supplement folic acid for individuals with MTHFR gene variants, who may have a reduced effectiveness to convert folic acid to the active L-methylfolate.⁶
Iron: Ferrous Sulfate vs. Iron Bisglycinate
⦁ Ferrous sulfate is commonly used in iron supplements but can cause nausea, constipation, diarrhea and abdominal pain.⁷
⦁ Iron bisglycinate has been shown to be up to 4x more bioavailable than ferrous sulfate and and has been associated with fewer gastrointestinal side effects.⁸⁻¹² Results from a meta-analysis showed that iron bisglycinate was more effective than other iron salts in increasing hemoglobin levels and reducing gastrointestinal adverse effects in pregnant women.⁷
Vitamin D: D2 vs. D3
⦁ Vitamin D3 (cholecalciferol) is more effective than Vitamin D2 supplementation (ergocalciferol), because D3 tends to raise blood levels more effectively.¹³
Key factors that influence bioavailability
Bioavailability isn’t just about choosing the right nutrient form—other factors significantly impact absorption:
Nutrient pairing: Some vitamins and minerals enhance each other’s absorption, while others compete:
⦁ Vitamin C promotes iron absorption.¹⁴⁻¹⁷
⦁ Vitamin D improves calcium uptake: Optimal vitamin D levels are necessary to increase the efficiency of calcium absorption. Without adequate vitamin D, the body absorbs no more than 10% to 15% of dietary calcium.¹⁸
Fat-soluble vs. water-soluble nutrients
⦁ Fat-soluble vitamins (e.g. A, D, E, K) require dietary fat for optimal absorption—taking them on an empty stomach reduces bioavailability.¹⁹
⦁ Water-soluble vitamins (e.g. C, B-complex) are absorbed more efficiently but aren’t stored long-term, requiring consistent intake.²⁰
Gut health & enzyme function:
a compromised gut microbiome or low stomach acid can significantly impair nutrient absorption.²¹
For example:
⦁ Iron: Low stomach acid can interfere with the conversion of iron (Fe³⁺) to a more absorbable form (Fe²⁺), potentially leading to iron deficiency.²²
⦁ B12: Low stomach acid can impair the absorption of vitamin B12, which is essential for nerve function and red blood cell production.²²
Individual Differences
⦁ Genetic variations e.g., MTHFR mutations affecting folate metabolism.
⦁ Lifestyle factors e.g., timing of supplementation, interaction with other foods and medications.
Bioavailability can be the difference between “taking” and “absorbing.”
Bioavailability isn’t just a buzzword—it’s a key determinant of whether micronutrient supplementation is actually effective. By considering nutrient interactions, delivery mechanisms, bioavailable forms and side effects, we can better ensure that what we consume translates into real health benefits.

Written By
The Land Lab Science Advisory Council

Review By
Hannah LaBrooy
MD, MPH
Dr. Hannah LaBrooy is a medical doctor and public health researcher with a multidisciplinary background spanning clinical medicine, public health, and international aid and development. She holds a Master of Public Health and previously worked as a Research Project Coordinator at the Kirby Institute (UNSW), contributing to publications in leading journals including The Lancet.
Her commitment to public health and equitable innovation was shaped by early experiences working in regional and remote drug and alcohol settings and a formative internship at The Grameen Bank in Bangladesh. Her professional and academic experience has focused on addressing health inequities, particularly in the area of access to care among marginalised populations.